Abstract
Introduction: Metabolic reprogramming of energy-generating pathways is a core oncogenic property of leukemias and other cancers that provides a potential therapeutic vulnerability.
In light of recent studies demonstrating reliance of Leukemia Initiating Cells (LIC) on OxPhos (Skrtic et al., 2011; Lagadinou at al., 2013), we aimed to determine the effects of OxPhosi on AML bulk and LICs in vitro and in vivo using patient-derived xenograft (PDX) AML models.
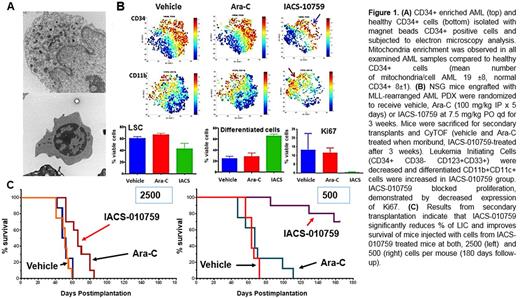
Methods and Results: Our gene set enrichment analysis conducted on publicly available gene expression profiles of LIC-enriched populations (Ng et al., 2016) confirmed significant enrichment of OxPhos-related genes relative to no LIC. Using transmission electron microscopy (TEM), we found a significant increase in mitochondria numbers in 8 primary CD34+ AML samples compared with 3 healthy bone marrow (hBM) CD34+ sample (19±8 vs 8±1,p=0.01, Fig. 1A), consistent with previously reported data (Škrtić at al.,2011). This finding provides rationale for assessing OxPhos as a potential target for therapeutic intervention.
IACS-010759 is a novel potent inhibitor of OxPhos (OxPhosi) that blocks cellular respiration through inhibition of mitochondrial complex I (Molina et al., AACR2016).
In 80% of the AML samples studied (n=50), IACS-010759 exposure induced profound growth-inhibitory effects in vitro at an EC50 of 3.1nM (0.1-11.7nM) and 5.0 nM (0.9-12.8nM) in AML blasts and CD34+ AML LIC respectively, with minimal toxicity against hBM CD34+ cells. In line with viability data, OxPhosi reduced colony forming ability of LIC (n=5, EC50 13-30nM) but not of hBM CD34+ cells. Further, IACS-010759 induces differentiation of CD34+ cells in a subset of AML samples as determined by flow cytometric analysis of colonies collected after treatment. Next, profound reduction of both, oxygen-dependent ATP production and spare respiratory capacity (SRC), at IC50s of 20.5 nM (range, 1.3*10-5 -528) for bulk and 51.4 nM (range, 1.3-528) for CD34+ cells, was shown by Seahorse assay. This translated into the mitochondrial membrane potential loss (TMRE, JC1 flow cytometry), mitochondria swelling and degeneration shown by TEM.
Based on genomic characteristics and responses to OxPhosi in vitro, two distinct groups of patients (pts) with unique metabolic pattern based on SRC were identified: samples from pts with low SRC (36.3±17.4 pmol/min) enriched in IDH1/2-mutated AML were sensitive to IACS-010759 with median 60% of viability drop at 123 nM, while samples with high SRC (86.7±20), enriched in TP53-mutated AML were resistant to OxPhosi with 30% viability reduction (p=0.03).
The proteome studies of AML pts samples revealed dose-dependent increased expression of energy stress response protein pAMPK, upregulation of glycolysis marker PFKFB and decrease of the fatty acids oxidation markers CPT1 and ACC1.
Further, the intracellular metabolome analysis of LIC from 4 primary AML pts showed modulation of amino acids (AA) with increased level of glutamine and aspartate, decreased TCA intermediates and increased lactate level indicative of OxPhos perturbation. In contrast, only moderate decrease of AA level and TCA intermediates was observed in hBM cells, consistent with lack of cytotoxicity on hBM. In a PDX model from MLL-rearranged AML refractory to standard chemotherapy, IACS-010759 treatment prolonged survival and delayed disease progression (Molina et al., AACR 2016). Mass cytometry analysis of BM and spleen cells demonstrated decrease of LIC (CD34+, CD38-, CD123+, CD33+), relative increase of CD11c+ differentiated cells and suppression of proliferation measured by Ki67 (Fig. 1B). The depletion of LIC by OxPhosi was confirmed in a secondary transplantation experiment. Mice injected with similar numbers of BM AML cells isolated from primary engrafted recipients of vehicle, Ara-C or IACS-010759 , showed improvement of the overall survival in OxPhosi arm (Fig. 1C).
Conclusion: Our study demonstrates that inhibiting OxPhos with IACS-010759 constitutes a novel promising therapeutic approach that targets a unique metabolic vulnerability of AML LICs via energy depletion, inhibition of proliferation and induction of differentiation. We have shown for the first time that IDH1/2 mutated AML have low spared respiratory capacity and are highly sensitive to IACS-010759. These findings are being tested in an ongoing Phase 1 clinical trial of IACS-010759 in AML (NCT02882321).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal